Overactive Bladder
Overview
Overactive Bladder, or OAB, is a bladder control problem characterized by uncontrollable urgency (the sudden compelling sensation to urinate that is difficult to put off). There is often frequency (urinating more than 8 times a day), or nocturia (waking more than once to urinate). There may or may not be urinary leakage. It affects both women and men equally, and is more common in older adults. The bladder serves to store urine and empty it; Overactive Bladder occurs because the muscles of the bladder start to contract involuntarily and erratically before it is full. These contractions can be difficult to control or stop, and may lead to incontinence.
OAB can affect your overall quality of life; you may feel embarrassed, isolated, and limited in your work and social life. We advocate various treatment options, from behavioral strategies and medication, to more advanced therapies. The ageing bladder is not like fine wine; it does not get better with age. However, a normal life is within your reach.
Some common causes include:
Overactive Bladder, or OAB, is a bladder control problem characterized by uncontrollable urgency (the sudden compelling sensation to urinate that is difficult to put off). There is often frequency (urinating more than 8 times a day), or nocturia (waking more than once to urinate). There may or may not be urinary leakage. It affects both women and men equally, and is more common in older adults. The bladder serves to store urine and empty it; Overactive Bladder occurs because the muscles of the bladder start to contract involuntarily and erratically before it is full. These contractions can be difficult to control or stop, and may lead to incontinence.
OAB can affect your overall quality of life; you may feel embarrassed, isolated, and limited in your work and social life. We advocate various treatment options, from behavioral strategies and medication, to more advanced therapies. The ageing bladder is not like fine wine; it does not get better with age. However, a normal life is within your reach.
Some common causes include:
- Advancing age
- Benign prostatic hyperplasia (BPH)
- Medications such as diuretics
- Neurological diseases such as stroke, Multiple sclerosis, and Parkinson’s disease
- Untreated diabetes
- Pelvic surgery & radiation
- Bladder stones & tumors
- Urinary Tract Infection
- Obesity
Tests
A complete medical history and evaluation is necessary to assess the scope of the problem. The work-up will usually include a:
Occasionally, specialized tests may also be performed including:
A complete medical history and evaluation is necessary to assess the scope of the problem. The work-up will usually include a:
- Urine test
- Blood work
- Bladder diary
Occasionally, specialized tests may also be performed including:
- Abdominal ultrasound: This test checks for abnormalities in the urinary system. It also determines how completely you empty your bladder.
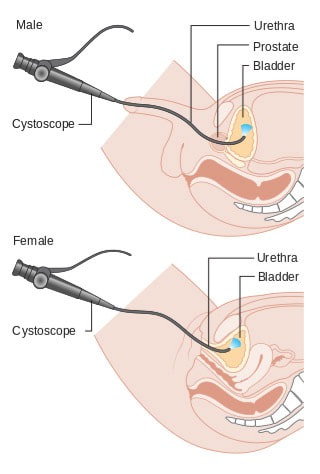
- Cystoscopy: This test evaluates the bladder for any abnormalities. A small scope called a cystoscope is inserted into the urethra to evaluate your urethra and bladder lining. It is used to visualize the urethra, prostatic urethra in men, bladder neck, and bladder. This will allow us to determine any abnormal findings including stones, masses, tumors, cancer, and foreign bodies. This is a painless office procedure.
Click here for more information
Treatments
There are many treatment options available to treat the symptoms of OAB. A stepwise approach is always best; often, simply lifestyle changes are sufficient, whereas some patients may need medical therapy in addition for greater success. For more complex cases, we are experts in advanced and surgical therapies.
Behavioral interventions are usually the first choice in treating OAB. These may include:
Medications are often prescribed in combination with lifestyle changes. They relax the bladder and can be helpful for relieving urgency, frequency, and urge incontinence. They may include:
More invasive therapies are available for those patients not getting satisfactory improvement with medication and behavior modifications. Additionally, some patients are unable to take medications due to side effects or other medical conditions.
Botox® may be injected into the bladder to block the muscles and nerves that lead to a feeling of urgently needing to urinate. The effects may last for up to 6-9 months, and repeated injections may be required. Risks include difficulty in emptying the bladder completely.
There are many treatment options available to treat the symptoms of OAB. A stepwise approach is always best; often, simply lifestyle changes are sufficient, whereas some patients may need medical therapy in addition for greater success. For more complex cases, we are experts in advanced and surgical therapies.
Behavioral interventions are usually the first choice in treating OAB. These may include:
- Pelvic floor exercises (often called Kegel exercises) which may help to strengthen the pelvic floor muscles and urinary outflow muscle used to hold back urine. A physical therapist specially trained in this area may be recommended. Results are not immediate, but it has been shown to give you more control of your urgency and help decrease leakage.
- Bladder diaries You are asked to keep track of when and how often you go to the bathroom. This helps us better understand how your symptoms affect you. It also brings awareness to what, when and how much you drink.
- Weight loss may ease your symptoms if you are overweight. Just an 8% decrease in body weight has been shown to have a 50% improvement in urinary symptoms.
- Fluid and diet management Avoidance of known bladder irritants and diuretics may improve symptoms for some people. The list includes caffeine, carbonated drinks, spicy foods, artificial sweeteners, alcohol, citrus, and chocolate. Modifying the timing and amount of fluid consumption may be helpful.
- Bladder training You may be able to break the urge to urinate by following a urination schedule rather than waiting until you have urgency. Begin with small delays when you feel the urge to urinate and gradually increase these until you are able to hold urine for more than 2 hours.
Medications are often prescribed in combination with lifestyle changes. They relax the bladder and can be helpful for relieving urgency, frequency, and urge incontinence. They may include:
- Anticholinergics/Antimuscarinics such as Vesicare® (Solifenacin), Enablex® (Darifenacin), Toviaz® (Fesoterodine), Detrol® (Tolterodine), and Oxybutynin in oral or gel form. Possible side effects are dry mouth, constipation, and dry eyes.
- Beta-3 Agonists such as Myrbetriq® (mirabegron) are a newer class of medicine that have an improved side effect profile, but may take longer to start working.
More invasive therapies are available for those patients not getting satisfactory improvement with medication and behavior modifications. Additionally, some patients are unable to take medications due to side effects or other medical conditions.
Botox® may be injected into the bladder to block the muscles and nerves that lead to a feeling of urgently needing to urinate. The effects may last for up to 6-9 months, and repeated injections may be required. Risks include difficulty in emptying the bladder completely.